Nominations Due February 26:
ASIPP Awards for Excellence in Pain Medicine Education & Leadership
The American Society of Interventional Pain Physicians (ASIPP) is accepting nominations for three distinguished awards recognizing excellence in pain medicine training, educational leadership, and emerging professional development. This is a reminder that nominations are due by Thursday, February 26.
These awards honor individuals and programs that embody comprehensive, ethical, and future-focused pain medicine practice.

Telehealth services extended through December 2027
The House and Senate have both passed and the President signed the federal spending package, which includes HHS funding and an extension of telehealth services through December 2027.
This legislation is effective retroactively as of February 1, 2026. As a result, there is no lapse in telehealth coverage that would have otherwise occurred following the January 31, 2026, expiration under the continuing resolution. In addition, the continuing resolution has been extended for an additional two weeks and continues to include telehealth services. We have been advised that there will be no disruption in telehealth reimbursement, and that all claims will be paid retroactively.
Please see the enclosed document for the specific legislative language included in the bill.
Extension of the telehealth provisions has been one of the major focuses of ASIPP’s efforts. Over the past several months, we have worked closely with Chairman Guthrie, Chairman Comer, and Chairman Cassidy to advance this initiative. ASIPP is very pleased to have secured this outcome—while mid-term rather than permanent, the two-year extension provides important continuity and stability. The language remains unchanged, with the extension being the primary modification, as outlined in the enclosed text.
Thank you for your continued assistance and cooperation. We also extend our sincere appreciation to our congressional supporters who helped make this significant achievement possible.

Telehealth services extended through December 2027
The House and Senate have both passed and the President signed the federal spending package, which includes HHS funding and an extension of telehealth services through December 2027.
This legislation is effective retroactively as of February 1, 2026. As a result, there is no lapse in telehealth coverage that would have otherwise occurred following the January 31, 2026, expiration under the continuing resolution. In addition, the continuing resolution has been extended for an additional two weeks and continues to include telehealth services. We have been advised that there will be no disruption in telehealth reimbursement, and that all claims will be paid retroactively.
Please see the enclosed document for the specific legislative language included in the bill.
Extension of the telehealth provisions has been one of the major focuses of ASIPP’s efforts. Over the past several months, we have worked closely with Chairman Guthrie, Chairman Comer, and Chairman Cassidy to advance this initiative. ASIPP is very pleased to have secured this outcome—while mid-term rather than permanent, the two-year extension provides important continuity and stability. The language remains unchanged, with the extension being the primary modification, as outlined in the enclosed text.
Thank you for your continued assistance and cooperation. We also extend our sincere appreciation to our congressional supporters who helped make this significant achievement possible.
Bibliometric Analysis of Musculoskeletal RFA Research Identifies Dr. Laxmaiah Manchikanti and Dr. Steven P. Cohen as Leading Authors, with Pain Physician and Pain Medicine Among the Most Influential Journals
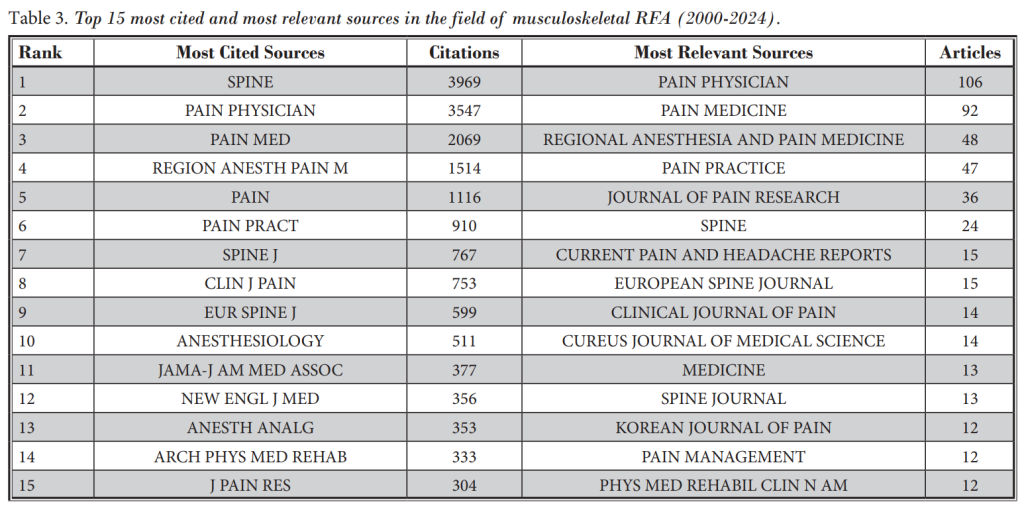
A recent article in Pain Physician titled “Radiofrequency Ablation for Musculoskeletal Pain: A Bibliometric Analysis of Global Research Trends (2000–2024)” (Pain Physician 2025; 28:S157-S168) examines the research landscape surrounding radiofrequency ablation (RFA) for musculoskeletal pain. The analysis identifies Pain Physician as the most relevant journal in this field, with Pain Medicine ranked as the second most relevant source.
Key findings and related bibliometric rankings include:
- Laxmaiah Manchikanti
- Identified as one of the most influential authors based on sustained productivity and citation impact, with contributions shaping the evidence base for spinal and genicular nerve interventions (Pain Physician 2025; 28:S157-S168)
- Ranked #1 globally for randomized controlled trials in chronic pain therapy spanning 1989–2024 (Medicine, 2025; 104:39)
- Ranked #1 among the most cited studies on epidural steroid injections (PM&R Sciences, 2025; 292-297)
- Dr. Steven P. Cohen
- Recognized for high citation impact and influence in musculoskeletal RFA research (Pain Physician 2025; 28:S157-S168)
For detailed data, please refer to the full article:
https://www.painphysicianjournal.com/current/pdf?article=ODA5Mg%3D%3D

Significant Medicare Physician Reimbursement Methodology Changes Finalized for 2026 with No Significant Changes for Ambulatory Surgery Center Payments
On October 31, 2025, the CMS issued a Final Rule that announces final policy changes for Medicare payments under the Physician Fee Schedule and other Medicare Part B issues effective on or after January 1, 2026.
Even though we have submitted numerous comments (ASIPP’s detailed comment letter), letters, and congressional requests, CMS has not made any changes in the Final Rule compared to the proposed rule. There are numerous misinterpretations, consequently resulting in errors to the payments.
PHYSICIAN PAYMENTS
Conversion Factor
- Beginning in January 2026, there will be two separate conversion factors (CF): one for qualifying alternative payment model (APM) participants (QPs) and one for physicians and practitioners who are not QPs.
- In 2026, the CF will be $33.57 for QPs and $33.40 for non-QPs. These amounts represent increases of 3.8% and 3.3%, respectively, compared to the 2025 CF of $32.35.
- The CF update is primarily based on three factors:
- A statutory update in the Medicare Access and CHIP Reauthorization Act that provides a 0.25% CF increase for non-QPs and 0.75% increase for QPs
- A 0.49% budget neutrality adjustment increase
- A one-time 2.5% increase due to the budget reconciliation legislation
Efficiency Adjustment
CMS finalized its proposal to apply an efficiency adjustment to non-time-based codes and services. As such, the agency will apply a negative 2.5% reduction to the work relative value unit (RVU) and the corresponding intraservice portion of physician time for non-time-based services. The efficiency adjustment will not apply to evaluation and management, care management, behavioral health, new codes, and any services on the Medicare Telehealth Services List.
Modifications to Indirect Practice Expense Methodology
CMS finalized its proposal to revise the methodology for allocating indirect practice expense (PE) costs for facility-based services by reducing the portion of facility PE RVUs by half the amount allocated to non-facility-based services. Previously, allocation was equal in both settings.
Indirect practice costs include expenses such as rent, administrative staff, scheduling, and billing and coding. CMS cites stakeholder concerns that paying both the physician and the facility for the same indirect costs may result in duplicative payment.
This shift in resources from facility to non-facility practices shifts reimbursement from one to the other. Non-facility practices will experience an increase in reimbursement while hospital-based practices will see a decrease in reimbursement.
Specialty Impact
As a result of these sweeping methodology reforms, on average, the interventional pain management specialty will experience a payment differential based on the physician’s practice setting.
- Physicians that practice in a facility setting (hospitals and ASCs) will see a reimbursement decrease of approximately 11%.
- Physicians in independent practices and office settings will see a reimbursement increase of approximately 7% to 10% for services provided in office settings, including procedures and E/M services.
- Unfortunately, for independent physicians providing services in ASCs, which is mistakenly considered as a facility as ASCs do not provide any benefits for practice expenses, there will be reimbursement decreases of 8% to 11% for any services provided in ASCs.
Telehealth
CMS finalized most telehealth policies as proposed:
- Streamlined Telehealth Services List: CMS will simplify the process for adding services to the list by removing the “provisional” and “permanent” distinction and focusing the review solely on whether the service can be effectively delivered via two-way audio-video.
- Removal of Frequency Limitations: Frequency limits for subsequent inpatient, subsequent nursing facility, and critical care consultation telehealth services will no longer be in place.
- Permanent Virtual Direct Supervision: For services requiring direct supervision, CMS will permanently allow this supervision to occur through real-time audio and visual interactive telecommunications (not audio-only).
The agency did revise the provision on the teaching physician policy and will allow teaching physicians to have a virtual presence in all teaching settings, in clinical instances when the service was furnished virtually, on a permanent basis.
Quality Payment Program (QPP)
CMS’ proposed rule limited changes to QPP in an attempt to provide stability to the program. As such, CMS finalized its proposal to keep the Merit-Based Incentive Payment System (MIPS) performance threshold at 75 points through the 2028 performance period/2030 MIPS payment year.
Ambulatory Specialty Model (ASM)
CMS has proposed the Ambulatory Specialty Model (ASM) to hold specialists financially accountable for managing chronic conditions in Original Medicare, focusing on low back pain and congestive heart failure. The model begins January 1, 2027, and runs through 2031, with payment adjustments starting in 2029.
Specialists—including anesthesiology, pain management, neurosurgery, orthopedics, and PM&R—would face payment adjustments from –9% to +9%, based on performance in disease management, adherence to clinical guidelines, and care coordination. However, CMS plans to use a “redistribution percentage” of 85%, ensuring Medicare savings by reducing total physician payments, unlike MIPS or the Hospital VBP program.
CMS refused to make any changes to Ambulatory Service Model for low back pain management as we have requested.
Summary of CMS Payment Rules
This summary highlights the good, bad and the ugly.
Good:
- Conversion factor increase of 3.6% to 3.8%.
- Payment increases of approximately 10% for office procedures and 7%–10% for evaluation and management (E/M) services.
- 2.6% payment increase for Ambulatory Surgery Center (ASC) services.
Bad:
- No permanent extension of telehealth services, despite multiple established rules. However, our sources indicate telehealth is included.
- A 2.5% efficiency adjustment applied to work RVUs for non-time-based services.
Ugly:
- 8%–10% reductions in physician payments for services provided in hospitals or ASCs. Our sources indicate telehealth is included.
In addition, physicians continue to face increasing administrative burdens, including preauthorizations, expanding Medicare regulations through LCDs (which are adopted by Medicare Advantage Plans, Medicaid, and incorporated into private medical policies), and frequent audits. At any given time, approximately 30% of interventional pain physicians are under audit. This has resulted in significant time spent on documentation, preauthorizations, and adherence to the appropriateness criteria set by LCDs and medical policies.
This is not a realistic assessment, given that physician payments have already decreased by 33% since 2001. The situation is further compounded by an ever-growing number of rules, regulations, and administrative burdens associated with EMRs—and now AI. Physician workload continues to rise, not fall. Remember the concept of “pajama time,” as many physicians work late into the evening to complete their documentation.
- The proposed conversion factor increase is only a temporary measure and may be clawed back, similar to the post-COVID cuts that followed payment increases under the Trump Administration.
- ASCs are being grouped with hospitals, despite being overwhelmingly owned and operated by independent physicians.
- ASCs essentially function as extensions of office practices.
- Independent physicians providing services at hospitals and ASCs are inaccurately classified as hospital-based physicians.
ASIPP will be providing you with additional analysis and is considering providing a webinar to highlight the key changes in 2026 Physician Fee Schedule for interventional pain management community.
2026 Fee Schedules
2026 Final Physician Fee Schedule IPM Codes
2026 Proposed ASC Fee Schedule IPM Codes

The tentative funding deal to open the government back up through January 30, 2026. Part of the package includes language to extend the telehealth flexibility and apply it retroactively
Lawmakers in the Senate cut a deal Sunday evening to end a federal government shutdown, but the path ahead remained unclear given the lack of involvement of either the White House or Republican leadership in the House of Representatives.
Sunday evening’s 60-40 vote cleared the chamber’s filibuster threshold and puts the resolution on schedule for a vote Monday or early in the week. Democrats could still gum up the process, but many took Sunday’s development as a sign that the caucus’s moderates had firmly decided on a course.
Eight moderate Democrats got on board with an agreement backed by their GOP colleagues that would extend government funding through the end of January while further negotiations take place on a range of issues, including subsidies for Affordable Care Act health plans, multiple news outlets reported Sunday evening.
The tentative funding deal to open the government back up through January 30, 2026. Part of the package includes language to not only extend the telehealth flexibility but also apply it retroactively.
The bipartisan agreement struck by moderate lawmakers on Nov. 9 is now on track for full approval this week in Congress. That vote will likely take place in the second week of December.
A summary of the bill can be found here:

Call to Action – Public Comments on Proposed LCD for
Peripheral Nerve Blocks & Procedures for Chronic Pain
UPDATE: For your convenience, we have created a petition for you, your staff, and patients to sign. We will compile the signatures and send the letter to all Medicare Directors. Just click on the link below to sign onto the petition and make your voice heard.
You must sign by Monday, November 8 in order to meet the comment deadline.
CLICK HERE TO SIGN THE PETITION
Last night, Thursday, October 23 ASIPP held a “Town Hall Meeting” for members who wanted more information on the proposed LCD for peripheral nerve blocks and pain procedures. Please click on the following link to view the presentation.
The news isn’t good folks! ASIPP has sent our comment letter on behalf of the society and our members. It is critical that you take the time to send a comment letter to your respective Medicare Administrator. We cannot stress strongly enough the importance of your action on this matter. Our specialty and patient care is at stake.
For your convenience, we are providing the email address and LCD number for each Medicare Administrator Contractor (MAC). Feel free to write your own comment letter, however if you would prefer, you can use the sample letter we have provided you. If you are unsure of which MAC covers your region/state, click here for a list.
CGS Administrators, LLC
(DL40261)
[email protected]
National Government Services, Inc.
(DL40267)
[email protected]
Noridian Healthcare Solutions, LLC
(DL40265)
[email protected]
Palmetto GBA
(DL40263)
[email protected]
WPS Insurance Corporation
(DL40300)
[email protected]

UPDATE: Medicare Administrative Contractors (MACs) to lift the claims hold and process claims with dates of service October 1, 2025, and later
This afternoon, CMS released the below updated guidance, directing all Medicare Administrative Contractors (MACs) to lift the claims hold and process claims with dates of service October 1, 2025, and later for services affected by the expiration of temporary payment provisions under the Full-Year Continuing Appropriations and Extensions Act, 2025 (P.L. 119-4). This includes claims under the Medicare Physician Fee Schedule, ground ambulance services, and Federally Qualified Health Center (FQHC) claims. MACs will also process telehealth claims that can be confirmed as behavioral or mental health services, while continuing to hold other telehealth and Hospital Care at Home claims pending further guidance.
Practitioners providing services no longer payable by Medicare should consider issuing an Advance Beneficiary Notice of Noncoverage (ABN). Clinicians participating in eligible Medicare Shared Savings Program ACOs may continue furnishing covered telehealth services without geographic restrictions under section 1899(l) of the Social Security Act.
CMS announces most payments to physicians will be paid “in a timely manner” except for telehealth and certain other services, as government shutdown continues
A revised CMS notice issued on October 15, 2025, stated that claims under the physician fee schedule and other payment programs will continue to be processed and paid on time. The only exceptions are claims associated with expired programs, such as telehealth flexibility. In reversing its earlier guidance, CMS clarified that payment holds will apply only to claims related to programs that have lapsed.
The revised notice reads:
“Effective October 1, 2025, CMS instructed all Medicare Administrative Contractors (MACs) to hold claims with dates of service of October 1, 2025, and later for services impacted by the expired Medicare legislative payment provisions passed under the Full-Year Continuing Appropriations and Extensions Act, 2025. Considering the continuing government shutdown, CMS will continue to process and pay held claims in a timely manner except for select claims for services impacted by the expired provisions. To date, no payments have been delayed as statute already requires all claims to be held for a minimum of fourteen days, and this recent hold is consistent with that statutory requirement. Providers may continue to submit claims accordingly.”
The ongoing government shutdown, which began on October 1, stems largely from disagreements over health care funding. Democrats are refusing to support a short-term spending bill unless it includes an extension of the enhanced Affordable Care Act (ACA) subsidies—expanded during the COVID-19 pandemic and set to expire at year’s end.
President Trump and Republicans, meanwhile, are pushing for a “clean” continuing resolution that maintains current funding levels through mid-November while deferring debate on health policy issues.

Medicare Releases Proposed LCD on Peripheral Nerve Blocks and Procedures for Chronic Pain With Elimination of Almost All Peripheral Nerve Blocks From Coverage Policy
All Medicare Administrative Contractors (MACs), including CGS, NGS, Noridian, Palmetto, and WPS, except Novitas and First Coast Service Options, have released new Local Coverage Determinations (LCDs) for peripheral nerve blocks and procedures for chronic pain.
The new LCDs provide coverage only for radiofrequency neurolysis for trigeminal neuralgia, corticosteroid injections for median neuropathy at the wrist (limited to a maximum of three injections), and corticosteroid injections for Morton’s neuroma (limited to a maximum of two injections).
All other peripheral nerve block and related procedures are not covered under these policies.
- Occipital nerve block and denervation
- Stellate ganglion block
- Trigeminal nerve block
- Suprascapular nerve block
- Thoracic nerve block
- Thoracic nerve denervation
- Genicular nerve blocks (GNB), cryoneurolysis or ablation
- Pudendal nerve block
- Digital nerve block
- Posterior tibial nerve block at the tarsal tunnel
- Ulnar nerve block
- Denervation of the trigeminal nerve for any diagnosis other than TN
- Any other peripheral nerves blocks, or denervation not listed above
This policy eliminates all procedures except for facet joint interventions and epidural interventions.
As practitioners, we recognize the clinical importance of these procedures. However, they are not performed very frequently, making it surprising that such a restrictive policy has been proposed—one that effectively removes nearly all other interventional options.
ASIPP will be submitting a formal comment letter and is urging all state societies to do the same.
Public comments are open until November 8 for CGS, NGS, Noridian, and Palmetto, and until November 22 for WPS.
Comments may be submitted directly through each Medicare Administrative Contractor (MAC) by using the links provided below:
NGS (DL40267):
Open Comment Period: closes 11/8
Noridian (DL40265):
Open Comment Period: closes 11/8
Palmetto (DL40263):
Open Comment Period: closes 11/8
CGS (DL40261):
Open Comment Period: closes 11/8
WPS (DL40300):
Open Comment Period: closes 11/22
We will stay in touch and provide you with a copy of the ASIPP letter. You will receive ASIPP’s official comment letter, which you can use as a reference to develop your own. However, if you would like to submit your letter before then, please feel free to do so.
When preparing your letter, please follow the principles below:
- Be respectful.
- Identify yourself and your practice.
- Clearly express your concerns.
- Offer solutions, if applicable. Possible recommendations include:
- Withdraw the LCD entirely.
- Modify coverage policies to allow two diagnostic blocks followed by two radiofrequency neurotomy procedures per year, if applicable, or four therapeutic nerve blocks.
- The treatment should be performed only if patients experience at least 50% improvement following both the first and second diagnostic blocks.
- Conclude your letter by thanking the MAC for their consideration.
- Keep in mind that the LCD itself includes detailed background information for each procedure.
- You may also reference supporting literature, either external sources or citations included within the LCD.

35-Year Analysis of Global Chronic Pain Trials Highlights Dr. Laxmaiah Manchikanti as Most Published Author and the Pain Physician Journal Takes Third Place
A 35-year bibliometric analysis of global trends in randomized controlled trials for chronic pain therapy (1989-2024) highlights Laxmaiah Manchikanti, MD, as a prominent author with the highest publication counts, while Pain Physician ranks as the third highest ranked journal. ASIPP Lifetime Director, Vijay Singh, MD, was also ranked in the top 10
The study, conducted by Yang et al., analyzed 4,206 publications from 939 journals, authored by 20,068 individuals across 86 countries. The most cited article was “Clinical Importance of Changes in Chronic Pain Intensity Measured on an 11-Point Numeric Pain Rating Scale” (Pain. 2001 Nov;94(2):149-158).
Most Published and Cited Authors:
- Laxmaiah Manchikanti, MD
- Andrew R. Moore, DSc
- Derry Sheena, MA
Top cited high-impact journals include:
- Pain
- Cochrane Database of Systematic Reviews
- Pain Physician
The tables below summarize:
- Publication and citation profiles of high-impact authors

- Bibliometric indicators of high-impact journals

For detailed data, please refer to the full article: https://journals.lww.com/md-journal/fulltext/2025/09260/global_trends_and_hotspots_of_randomized.107.aspx

Update on Medicare Operations: Telehealth, Claims Processing, and Medicare Administrative Contractors Status During the Shutdown
When certain legislative payment provisions (“extenders”) are scheduled to expire, CMS directs all Medicare Administrative Contractors (MACs) to implement a temporary claims hold. This standard practice is typically up to 10 business days and ensures that Medicare payments are accurate and consistent with statutory requirements. The hold prevents the need for reprocessing large volumes of claims should Congress act after the statutory expiration date and should have a minimal impact on providers due to the 14-day payment floor. Providers may continue to submit claims during this period, but payment will not be released until the hold is lifted.
Absent Congressional action, beginning October 1, 2025, many of the statutory limitations that were in place for Medicare telehealth services prior to the COVID-19 Public Health Emergency will take effect again for services that are not behavioral and mental health services. These include prohibition of many services provided to beneficiaries in their homes and outside of rural areas and hospice recertifications that require a face-to-face encounter. In some cases, these restrictions can impact requirements for meeting continued eligibility for other Medicare benefits. In the absence of Congressional action, practitioners who choose to perform telehealth services that are not payable by Medicare on or after October 1, 2025, may want to evaluate providing beneficiaries with an Advance Beneficiary Notice of Noncoverage. Practitioners should monitor Congressional action and may choose to hold claims associated with telehealth services that are not payable by Medicare in the absence of Congressional action. Additionally, Medicare would not be able to pay some kinds of practitioners for telehealth services. For further information: https://www.cms.gov/medicare/coverage/telehealth.
CMS notes that the Bipartisan Budget Act of 2018 allows clinicians in applicable Medicare Shared Savings Program Accountable Care Organizations (ACOs) to provide and receive payment for covered telehealth services to certain Medicare beneficiaries without geographic restriction and in the beneficiary’s home. There is no special application or approval process for applicable ACOs or their ACO participants or ACO providers/suppliers. Clinicians in applicable ACOs can provide these covered telehealth services and bill Medicare for the telehealth services that are permissible under Medicare rules during CY 2025, irrespective of further Congressional action. For more information: https://www.cms.gov/files/document/shared-savings-program-telehealth-fact-sheet.pdf.
MACs will continue to perform all functions related to Medicare Fee-for-Service claims processing and payment.
ASIPP Files Comments to CMS on Physician Fee Schedule: ASIPP Requests Elimination of Cuts, Introduction of a Modifier for Independent Physicians
CMS issued the proposed rule CMS-1832-P on July 16, 2025, titled Medicare and Medicaid Programs; CY 2026 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; and Medicare Prescription Drug Inflation Rebate Program.
On September 11, 2025, ASIPP submitted a comment letter advocating for the following:
- Elimination of proposed efficiency adjustment, which is inappropriate, and efficiency is rather decreasing than increasing.
- Due to escalating costs, practice expense cuts applicable to independent physicians need to be addressed.
- Ambulatory Specialty Model (ASM) appears to be without evidence and inappropriate, putting independent physicians at high risk for survival; consequently, this should be eliminated or conducted voluntary trial for five years.
- Telehealth services must be made permanent.
Enclosed are ASIPP’s detailed comment letter, Chairman Comer’s recent letter to CMS and OMB, and 3 published articles addressing this issue.
- Manchikanti L, et al. Physician payment reform in interventional pain management: Balancing cost, quality, access and survival of independent practices. Pain Physician 2025; in press.
- Manchikanti L, et al. Non-partisan proposal for reforming physician payment system and preserving telehealth services. Pain Physician 2025; 28:E329-E335.
- Manchikanti L, et al. Escalating growth of spending on Medicare Advantage (MA) plans: Save Medicare from insolvency and balance the budget. Pain Physician 2025; in press.

Aetna and Cigna Announce Automatic Downcoding Policies
Background
- Aetna and Cigna have announced automatic downcoding policies for complex Evaluation & Management (E/M) services — specifically, level 4 and level 5 office visits.
- Aetna and Cigna are using algorithms or claims data alone to automatically downgrade the codes physicians assign to cases — without reviewing individual patients’ medical records.
- The result is that claims for complex visits will be paid at a lower level. Physicians who disagree with this automatic downcoding will have to appeal.
- That process will require submitting a significant amount of paperwork and patient case documentation — something many practices will not have the capacity or wherewithal to do.
- This “deny first, pay later” system presumes physicians are guilty of “upcoding” until proven innocent.
Issues we are facing:
- These new policies from Aetna and Cigna do not put patients first. They’re not about catching bad actors. They’re about boosting insurer profits at the expense of patient access and timely care.
- These policies threaten the viability of independent physician practice. Automatic downcoding will accelerate the collapse of independent practices that communities rely on for accessible, affordable care.
- Insurers are acting in bad faith. Aetna and Cigna are rewriting the rules of medical coding unilaterally, disregarding physician expertise and nationally recognized standards.
Potential Scope of the Policy
- Aetna and Cigna’s policies will have the potential to impact some of the most commonly billed codes
- According to CMS data of Medicare Part B E/M codes by specialty in CY 2022, E/M CPT code 99214 was the most frequently billed E/M code (of 114 codes tracked), representing 25% of allowed E/M claims. E/M CPT code 99215 was the sixth most frequently billed E/M code in the same data set, representing 3% of all codes billed.
- Overcoding of CPT codes 99214 and 99215 is de minimis
- According to a 2024 audit of Medicare FFS claims, CPT codes 99214 and 99215 overcoding represented 0.13% of paid Medicare FFS claims in 2024.
- Cigna anticipates that this new policy will affect less than 3% of eligible claims.
* This is a significantly greater percentage of claims than CMS data would suggest are actually overcoded
- When you consider the high volume of claims this would affect, and the low likelihood that they are incorrectly coded, it is difficult to justify this policy as anything more than a way for insurers to erect even more barriers to paying physicians for the services they have already provided
Effect on Patients
- These policies will force physicians to spend even more time doing paperwork that would have been better spent treating patients.
- Instead of treating patients, physicians will have to spend their time fighting the likes of Aetna and Cigna for just reimbursement.
- Aetna and Cigna are putting patients in the middle of a claims tug-of-war.
- Aetna and Cigna are using mysterious, opaque algorithms to second-guess the clinical judgment of the physicians that patients trust — and refusing to explain or justify their decisions.
Effect on Independent Physicians
- Independent practices lack the armies of coders and administrators that hospital systems have. They don’t have the capacity to play insurers’ bureaucratic games.
- Downcoded claims necessitate time-consuming appeals and effectively force practices to beg for payment for the care they’ve provided.
- A policy of automatic underpayment strains independent practices’ scarce resources.
- And by threatening independent practices’ financial viability, these policies hasten consolidation within the healthcare market.
- To avoid these administrative and financial headaches, independent practices accede to buyout offers from large hospitals and health systems.
- Such consolidation results in higher costs, fewer choices, and less personalized care for patients.
Backward Policy
- Both policies flout coding guidelines from the American Medical Association and the Centers for Medicare and Medicaid Services, which require review of medical records to determine visit complexity.
- Aetna and Cigna’s approach is opaque. Physicians do not know the criteria or algorithms being used, leaving them unable to avoid downcoding even if they code correctly.
- These actions may even conflict with federal and state law, including prompt-pay requirements and fair claims review standards.
Please find policies linked below:

Congress Moves to Extend Telehealth Access Through 2027
Bipartisan and bicameral bills have been introduced to extend telehealth access through fiscal year 2027.
Telehealth services have become a crucial part of modern medical practice, especially since the COVID-19 pandemic. They provide numerous benefits to patients, helping to address issues like transportation barriers, missed work for caregivers, and financial strains. Medicare has played a key role in expanding access to telehealth, benefiting not only rural Americans but also the broader population, as most insurers—except United Healthcare Commercial— have adopted these policies.
The Telehealth Modernization Act of 2025, led by Reps. Buddy Carter (R-GA) and Debbie Dingell (D-MI), ensures continued access to telehealth services for seniors and patients nationwide. A companion bill is being advanced in the Senate by Sens. Tim Scott (R-SC) and Brian Schatz (D-HI).
Lawmakers emphasized the critical role of telehealth in reducing barriers to care, improving access for rural and underserved patients, and modernizing healthcare delivery.
This legislation represents a major step toward securing long-term telehealth access for Medicare patients and strengthening its place in the U.S. healthcare system.

Requesting support to CMS and Congressional Members to Revise Proposed Physician Payment Rule to Separate the Cuts Applied for Hospital-Based Physicians from Independent Physicians
ASIPP is advocating strongly on behalf of interventional pain physicians, sending letters to Congress urging revisions to the proposed 2025 Physician Payment Rule from the Centers for Medicare & Medicaid Services (CMS). While ASIPP supports CMS’s goals of reducing waste, improving quality, and strengthening chronic disease management, the current proposal would have devastating consequences for interventional pain practices. These sweeping cuts risk accelerating healthcare consolidation, reducing patient access to pain specialists, and worsening physician burnout, at a time when practice costs are soaring, staff wages are rising, and reimbursement rates continue to fall.
Since 2001, interventional pain physicians have experienced some of the steepest cuts across all specialties, 41% through 2025, projected to reach 45% with the new rule. Even with modest office-based payment relief projected for 2026, the cumulative losses remain unsustainable.
In addition, CMS is introducing an Ambulatory Specialty Model (ASM) that will begin a trial phase in select states starting January 2027 and continue for five years through December 31, 2031.
This pilot will focus on two chronic conditions, low back pain and heart failure, with the following objectives:
- Prevent the worsening of chronic conditions
- Identify risks and early signs of chronic conditions
- Improve patient experience
- Reduce unnecessary procedures and surgeries
The specialties included are interventional pain management, anesthesiology, neurosurgery, orthopedic surgery, and physical medicine and rehabilitation. During the first payment year, adjustments will range from -9% to +9%, with all participants subject to this risk. Participation is mandatory, not optional.
However, there is no established or evidence-based guidance for this model, which significantly increases the risk for pain specialists. Pain specialists do not manage acute pain and have no control over many of the associated costs, yet they would still be held accountable for overall patient spending. These payment adjustments may apply to all Medicare services.
ASIPP urges CMS to eliminate the ASM until appropriate criteria are established and the model’s effectiveness is demonstrated.
ASIPP is urging Congress to:
- Reverse the proposed 2.5% efficiency adjustment to work RVUs and stop the cycle of devastating cuts every three years.
- Promote equitable treatment of independent pain practices in practice expense allocations, especially for services provided in Ambulatory Surgery Centers.
- Ensure the permanent extension of telehealth access beyond 2025, critical for chronic pain patients in rural and underserved areas.
- Direct CMS to distinguish reimbursement reductions between hospital-employed and independent physicians, protecting small pain practices from disproportionate harm.
- Ask CMS to withdraw this provision pending the development of appropriate criteria and validation of the model’s effectiveness.
Without these revisions, independent interventional pain practices, already under audit pressure and burdened by prior authorization requirements, face an uncertain future. Preserving their viability is essential to maintain patient access to timely, high-quality pain care and to prevent further healthcare consolidation that continues to drive up costs by 200–300%.
SAMPLE LETTER TO SEND TO REPRESENTATIVES IN CONGRESS
ASIPP has prepared a sample letter you can personalize and send to your representatives in Congress.
Click here to find your congressional members
By speaking out, you can help stop devastating cuts, protect independent interventional pain practices, and preserve patient access to high-quality pain care.
Please click here for a sample letter to send to your representatives.
SAMPLE LETTER TO SUBMIT COMMENTS TO CMS
For your convenience, we are enclosing a sample letter for you to customize and send to CMS to express concerns with the 2025 Medicare Physician Fee Schedule.
Please click here for a sample letter to submit your comments to CMS.
INFORMATION FOR SUBMITTING YOUR COMMENT LETTER
In commenting, please refer to file code CMS-1832-P. Comments must be received no later than 5 p.m. on September 12, 2025.
Click here to submit electronic comments on this regulation.
Please do not hesitate to contact us if you have any questions or would like additional information.
Thank you,
Laxmaiah Manchikanti, MD
Chairman of the Board and Chief Executive Officer, ASIPP and SIPMS
[email protected]
Mahendra Sanapati, MD
ASIPP President
[email protected]

Non-Partisan Proposal for Reforming Physician Payment System and Preserving Telehealth Services
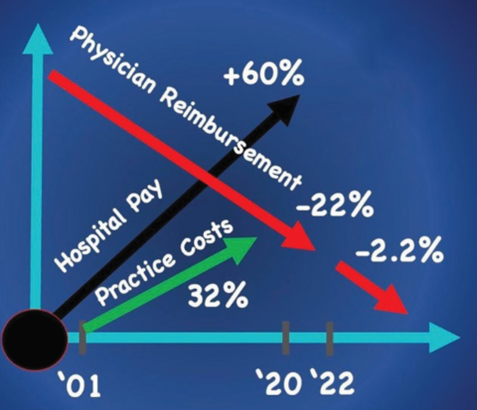
Physician payments have declined significantly due to budget neutrality rules and reimbursement cuts. Since 2001, Medicare payments to physicians have dropped by 33% when adjusted for inflation. These reductions have been compounded by 2% annual sequestration cuts introduced after the Affordable Care Act (ACA), which continues through 2032. Despite their long-term impact, sequestration cuts receive little public attention.
Congress has historically delayed or softened these cuts. However, in 2025, a bill that would have adjusted payment rates was removed from the continuing resolution, resulting in continued reductions. Meanwhile, insurance premiums have risen nearly 400%, highlighting the disparity between healthcare costs and physician compensation.
Ironically, while physicians face significant payment cuts, the Centers for Medicare & Medicaid Services (CMS) proposed on January 10, 2025, a 4.3% payment increase for Medicare Advantage plans—totaling $21 billion in 2026 and an estimated $210 billion over the following decade starting in calendar year 2026. This proposal comes amid ongoing concerns about Medicare Advantage overpayments, estimated at nearly $100 billion annually, and additional funding through annual premiums of $198 from all Medicare beneficiaries, amounting to roughly $13 billion per year.
In response, the American Society of Interventional Pain Physicians (ASIPP) submitted a nonpartisan reform proposal advocating for telehealth protections and elimination of sequester cuts—measures that have received strong bipartisan support in Congress.
Both the House of Representatives and the Senate voted to pass a reconciliation bill—nicknamed the “Big Beautiful Bill”, which has been signed into law by the President recently. It proposes an $8.9 billion investment in the Medicare Physician Fee Schedule, with a 2.25% update in 2026.
The proposal does not address the budget neutrality provision, growing practice costs, inflationary pressures, or ongoing sequestration and pay-as-you-go (PAYGO) cuts. It also fails to resolve issues with the Medicare Access and CHIP Reauthorization Act (MACRA), particularly within the Merit-Based Incentive Payment System (MIPS).
On November 1, 2024, CMS finalized a 2.8% cut to physician payments—an estimated $20 billion—while also eliminating telehealth services. These cuts continue to threaten physician sustainability and patient access to care.
📄 Read the full Pain Physician Journal article here → https://www.painphysicianjournal.com/current/pdf?article=ODAyNA%3D%3D

IMPORTANT NEWS!
Medicare Physician Fee Schedule & Ambulatory Surgery Center Rule
CMS proposes a 3.8% payment increase for physicians, the first in 5 years, along with a 2.6% increase for ASC payments and an 8%–10% increase for office-based services. However, payments for hospital and ASC-based physician services are reduced by 8%–10%.
PHYSICIAN PAYMENTS
On July 14, 2025, the Centers for Medicare & Medicaid Services (CMS) released the proposed rule for the Calendar Year (CY) 2026 Medicare Physician Fee Schedule (PFS). The rule introduces significant changes to physician payment policies and updates to the Quality Payment Program (QPP), including the Merit-based Incentive Payment System (MIPS) and Alternative Payment Models (APMs).
KEY PROPOSED CHANGES:
1. Conversion Factor (CF) Updates
- Proposed Conversion Factor Increase:
- The proposed conversion factor for qualifying participants (QPs) is $33.59 (a 3.83% increase from 2025), and for non-QPs, it is $33.42 (a 3.62% increase).
- These increases reflect a one-time 2.5% statutory payment adjustment from the One Big Beautiful Bill Act, in addition to other updates.
- ASIPP’s Comments:
- ASIPP welcomes the proposed increases but cautions that much of the adjustment is temporary, raising concerns about potential future pay cuts. ASIPP continues to advocate for a permanent inflationary adjustment and the elimination of budget neutrality constraints. Notably, ASIPP has submitted a nonpartisan proposal to reform Medicare physician payments, which includes a permanent fix and the elimination of the 2% sequestration cuts (https://asipp.org/draft-drm-non-partisan-proposal-for-reforming-2/).
We are already experiencing clawbacks from increases provided during the COVID-19 pandemic under the Trump Administration, with ongoing rulemaking leading to a 2.8% cut for 2025. Furthermore, the 2% sequestration cut, originally intended to expire years ago, has now been extended until 2031.
2. Efficiency Adjustment
- Purpose: CMS proposes a new -2.5% efficiency adjustment for non-time-based codes, applied every 3 years.
- CMS Rationale: This adjustment reflects concerns about potentially overestimated time assumptions and aims to account for increasing physician efficiency.
- ASIPP’s Comments: ASIPP supports initiatives that encourage efficiency; however, applying a reduction in work value for perceived efficiency gains is inappropriate. Despite advancements in EMRs and AI, administrative burdens have only increased, leading to greater stress rather than relief.
Additionally, physicians face growing challenges with preauthorizations, expanding Medicare regulations (including LCDs), and cascading requirements from Medicare Advantage Plans, Medicaid, and private insurers. These are compounded by ongoing audits, with approximately 30% of interventional pain physicians under audit at any given time. IPM physicians are dedicating significant time to documentation, preauthorizations, and compliance with LCDs and medical policies. As such, a 2.5% reduction in work value, without accounting for inflation or the cumulative 33% reduction in physician payments from 2001 to 2025, raises serious concerns.
3. Practice Expense (PE) Methodology
- Proposed Change: CMS proposes reducing the portion of indirect PE for facility-based services, citing outdated assumptions and the increasing trend toward hospital employment.
- CMS Rationale: The goal is to discourage hospital consolidation and promote payment parity across care settings.
- Impact: This proposal could result in approximately 10% total RVU reductions for facility-based (hospital and ASC) interventional pain management (IPM) services.
- ASIPP’s Comments: ASIPP is deeply concerned about the negative impact on independent practices. There must be an appropriate methodology to address this issue. The vast majority of physicians practicing in ASCs—and many non-primary care independent practitioners—also provide care in hospital settings. Importantly, many procedures cannot be performed in office settings, and not all physicians are equipped to offer these services outside ASCs. In many cases, Ambulatory Surgery Centers effectively serve as an extension of a physician’s office. ASIPP urges CMS to revise this policy by distinguishing between procedures performed in ASCs and those in hospital settings, and by implementing a methodology to differentiate independent physicians from hospital-based physicians.
4. Telehealth
- No proposed extension: CMS’s proposed rule does not provide any evidence or statements supporting a permanent extension of telehealth services.
- CMS proposed changes: However, CMS does propose permanent changes such as a revised definition of “direct supervision.”
- Our sources at CMS indicate that telehealth is included in the 2026 physician fee schedule.
BRIEFLY:
ASIPP analysis indicates that office payments, including physician payments, for procedures and evaluation and management (E/M) services are expected to increase by approximately 10%.
Conversely, payments to physicians for services performed in hospitals or ASCs, whether by independent or hospital-based physicians, are projected to decrease by about 8%, including reductions to E/M services.
SUMMARY OF PHYSICIAN PAYMENT REFORM
2026 Proposed – Physician Payment Rates Compared to 2025 (https://asipp.org/2026physicians_proposed/)
2026 AMBULATORY SURGERY CENTER RULE
The Centers for Medicare & Medicaid Services (CMS) has proposed a 2.4% payment increase for Ambulatory Surgical Centers (ASCs) in the CY 2026 payment rule. This increase is contingent upon ASCs meeting quality reporting requirements. Additionally, CMS proposes significant expansions to the ASC Covered Procedures List (ASC-CPL), allowing a broader range of procedures to be performed in ASCs.
Payment Rate Increase:
- CMS proposes a 2.4% payment increase for both Ambulatory Surgery Centers (ASCs) and Hospital Outpatient Departments (HOPDs).
- This increase reflects a 3.2% market basket update, offset by a 0.8% productivity adjustment—consistent with the Inpatient Prospective Payment System (IPPS) update factor.
2026 ASC Proposed Payment Rates Compared to 2025 Rates https://asipp.org/2026asc_prposed/)
SUMMARY OF CMS PAYMENT RULES
This summary highlights the good, the bad and the ugly.
Good:
- Conversion factor increase of 3.6% to 3.8%.
- Payment increases of approximately 10% for office procedures and 7%–10% for evaluation and management (E/M) services.
- 2.6% payment increase for Ambulatory Surgery Center (ASC) services.
Bad:
- No permanent extension of telehealth services, despite multiple established rules. However, our sources indicate telehealth is included.
- A 2.5% efficiency adjustment applied to work RVUs for non-time-based services.
Ugly:
- 8%–10% reductions in physician payments for services provided in hospitals or ASCs. Our sources indicate telehealth is included.
In addition, physicians continue to face increasing administrative burdens, including preauthorizations, expanding Medicare regulations through LCDs (which are adopted by Medicare Advantage Plans, Medicaid, and incorporated into private medical policies), and frequent audits. At any given time, approximately 30% of interventional pain physicians are under audit. This has resulted in significant time spent on documentation, preauthorizations, and adherence to the appropriateness criteria set by LCDs and medical policies.
This is not a realistic assessment, given that physician payments have already decreased by 33% since 2001. The situation is further compounded by an ever-growing number of rules, regulations, and administrative burdens associated with EMRs—and now AI. Physician workload continues to rise, not fall. Remember the concept of “pajama time,” as many physicians work late into the evening to complete their documentation.
- The proposed conversion factor increase is only a temporary measure and may be clawed back, similar to the post-COVID cuts that followed payment increases under the Trump Administration.
- ASCs are being grouped with hospitals, despite being overwhelmingly owned and operated by independent physicians.
- ASCs essentially function as extensions of office practices.
- Independent physicians providing services at hospitals and ASCs are inaccurately classified as hospital-based physicians.
While ASIPP appreciates the positive changes, it continues to advocate for revisions to the fee schedule that distinguish independent physicians from hospital-based physicians. This distinction is critical to ensure that independent physicians working in hospitals and ASCs are not unfairly subjected to payment reductions intended for hospital-employed providers.
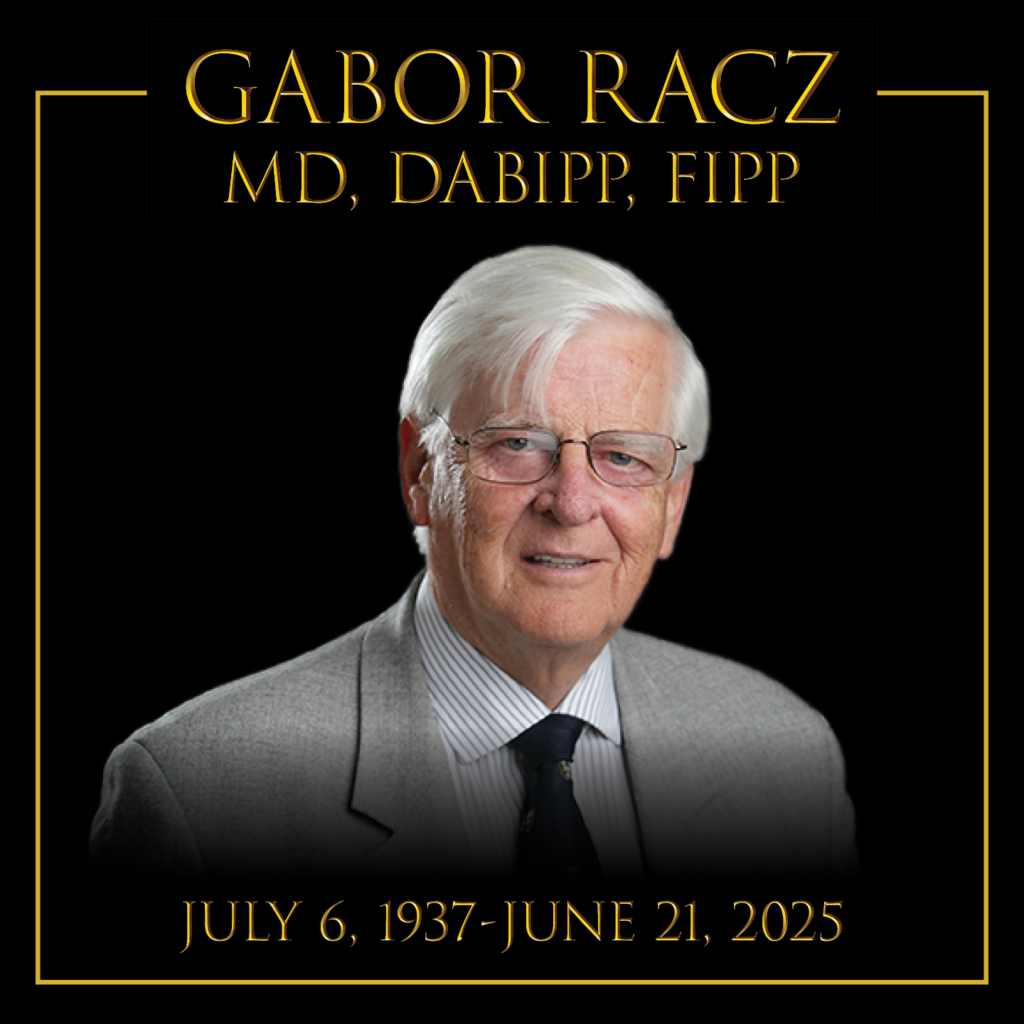
GABOR B. RACZ, MD, IN MEMORIAM
It is with profound sadness and a deep sense of loss that we share the passing of our beloved teacher, mentor, friend, and colleague, Gabor Bela Racz, MD, who passed away peacefully in his sleep in the early hours of June 21, 2025. Widely recognized as a Giant in pain management worldwide and awarded by the American Society of Interventional Pain Physicians (ASIPP) with this award, Dr. Racz’s contributions shaped the very foundation of our field.
Though he earned global acclaim, many of us remember him best as the long-serving Professor and Chair of Anesthesiology in Lubbock, Texas, where he trained hundreds of fellows and countless other physicians. He was an innovator at heart, pushing the boundaries of interventional pain medicine with vision and precision. I recall, even as early as 1982 when I began my anesthesiology practice, Dr. Racz had already pioneered the use of a spring, shear-resistant catheter to perform epidural injections in patients with epidural fibrosis—an innovation inspired by the kinking of an intravenous catheter in a pregnant patient. This eventually became the percutaneous epidural neuroplasty, known worldwide as the “Racz Procedure”, now performed hundreds of thousands of times across the globe.
His pioneering work extended beyond catheters and techniques. He applied this same catheter for intrathecal phenol injections for cancer pain and later combined it with hypertonic saline for adhesiolysis, further refining and standardizing these procedures.
Dr. Racz’s educational impact was equally far-reaching. Together with Dr. Prithvi Raj, he co-founded the World Institute of Pain (WIP), and the Annual Gabor Racz Pain Conference in Budapest stands as a testament to his enduring legacy.
He consistently emphasized that every procedure must be SAFE (safe, appropriate, fiscally responsible, and effective), he advanced multiple interventional techniques for both cancer and non-cancer pain, including early work in neuromodulation. Despite his towering influence across continents, it is humbling to remember that he began his life in Budapest (born 1937), fleeing Hungary during the 1956 Revolution with his beloved wife Enid, and later making the United States his home. He raised a loving family and found joy in the company of his children and grandchildren.
On a personal note, I first met Dr. Racz during a breakfast meeting—an encounter that led me to begin performing adhesiolysis. When I once faced a complication with a retained catheter, he personally guided me through the resolution. He had a gift for recognizing and encouraging original thinkers, and I was honored to receive the Trailblazer Award from him through WIP. I cherish the photographs from his visit to Paducah, KY, where he and Enid spent time with us, along with Drs. Prithvi and Susan Raj. These moments and memories hang proudly in my home and office.
Dr. Racz will be remembered not only for his unparalleled contributions to pain medicine but also for his compassion, mentorship, and enduring humanity. His absence leaves a void that will not be easily filled—but his legacy will live on through every life he touched and every procedure he refined.
While we miss him sorely, this is the time we can memorialize him. If you are interested in writing about him, please submit the manuscripts to Pain Physician. You will be waived the submitting fee.
Limits are as follows:
Abstract: Up to 250 words
Text: Maximum of 3,000 words
You can use pictures, references, etc. which are outside the limits.


Following Memoriam Provided by Standiford Helm, MD
Gabor Bela Racz, MD passed away peacefully in his sleep in the early hours of June 21, 2025. With his passing, we have lost one of the great figures of interventional pain management.
Dr. Racz was born and raised in Budapest. He left Budapest in the turbulent days of the 1956 Hungarian revolution with his wife of sixty-four years. One can still see the chip created in the building by a bullet intended for him.
Dr. Racz was able to make his way to England, where he completed his medical education and played on the English national water polo team. He was able to emigrate to the United States, where he started his academic career at Syracuse, NY. In 1977, he moved to Texas Tech, where he developed and ultimately led the pain program.
Dr. Racz’s academic career was characterized by ceaseless efforts to improve and innovate. A few weeks before his passing, his conversation focused on potential medical innovations and areas for new research. As early as 1976, he pioneered the use of spring-wound, shear-resistant catheter. Initially, this catheter was used to aid in the proper intrathecal placement of phenol for cancer. Coupling this development with an appreciation of the use of hypertonic saline, it was a short step to the creation of the percutaneous adhesiolysis procedure, whose shorthand name is the Racz procedure, done with a Racz catheter.
Dr. Racz’s educational efforts continued on an international scale. He was instrumental in developing the World Institute of Pain, which will be holding the 28th Annual Gabor Racz Pain Conference later this year.
Dr. Racz believed in the three pillars of interventional pain management, efficacy, safety, and patient access. He was always focused on how to change procedural techniques to avoid complications. The blunt needles whose use he pioneered changed the risk profile of arterial impingement.
Gabor Racz’s passion was his belief that no one should live in pain. He believed in his patients and was determined to support and heal them. He was more than a physician; he was their hero.
He said, “Treat your patient as if they were your own mother.”
BREAKING NEWS! Impact of One Big Beautiful Bill on Physician Payment Reform
The budget reconciliation package passed on Thursday, May 22, and included several provisions that would significantly impact physician payments and healthcare overall. Unfortunately, there is no unequivocally good news; rather, we are faced with a mix of potentially good, bad, and ugly developments.
Maybe Good News
Medicare Physician Fee Schedule Updates:
1. Initial Increase: The bill proposes a 2.25% Medicare pay update for physicians in 2026, based on 75% of the Medicare Economic Index (MEI), at a projected cost of $8.9 billion for that year.
Bad News
1. Future payment updates would be tied to the MEI, which tracks inflation and physician practice costs.
However, while linking payment updates to the MEI is a step in the right direction, concerns persist that the proposed MEI updates—capped at 10% annually—will not keep pace with actual inflation and rising practice expenses. This could result in effective increases of less than 0.5%.
2. The physician payment conversion factor is based on three components, including:
• An inflationary index, which is currently projected as 0% for 2025.
• A budget neutrality adjustment would apply solely to physician payments.
• Payments would continue to be influenced by the Merit-Based Incentive Payment System (MIPS). Consequently, CMS retains the authority to convert even minimal positive inflation adjustments into negative adjustments.
3. The continuation of 2% sequestration cuts, initially implemented after the Affordable Care Act, is set to extend through 2032.
4. Broader healthcare provisions will also affect physicians. These include Medicaid cuts, implementation of work requirements, and reductions in multiple assistance programs, which are likely to lead to decreased Medicaid enrollment.
What Is Ugly?
• What is particularly troubling is the ongoing instability of the physician payment system and the continued imposition of 2% sequestration cuts.
• Overall payment reductions could reach as high as 6%, despite the proposed MEI-based increases.
We find ourselves in a critical situation. ASIPP has long been engaged in addressing these challenges through a non-partisan proposal to reform the physician payment system and safeguard telehealth services. The bill is now before the Senate. Please contact your senator individually, through your group, patients, or staff—and urge them to support meaningful reform of the physician payment system. You may also use the convenient link set up by ASIPP: https://www.votervoice.net/ASIPP/Campaigns/127211/Respond

ASIPP Submits Letters to Carelon and Humana Regarding Coverage for Interventional Pain Management Procedures
BREAKING NEWS! ASIPP Submits Non-Partisan Reconciliation Proposal for Physician Payment Reform
Recently, ASIPP submitted to members of Congress, a non-partisan proposal for budget reconciliation for the preservation of Medicare and Medicaid and the reform of the physician payment system.
This proposal is in response to the escalation of health care spending in the United States, which in 2023 was close to $4.9 trillion, a 7.5% increase from the previous year the Congressional Budget Office (CBO), and other sources indicate that net Medicare spending—after accounting for beneficiary premiums—is projected to total $14 trillion over the next decade. Simultaneously, the financial sustainability of physician practices is increasingly under pressure.
Over the past 24 years, physician payment rates have declined by 33%, while practice costs have steadily risen. The cost of medical equipment, supplies, and technology has grown from $30.2 billion in 2017 to $57 billion in 2023, reflecting an average annual growth rate of 6.5%. The overall increase in practice expenses may be even greater, compounding the financial challenges faced by providers. Additionally, a widening gap has emerged: while physician payments have declined, other health care sector payments have continued to rise. Perhaps the most striking is the contrast between insurance premium growth and physician reimbursement rates, with premiums increasing nearly 400% while physician payments have dropped by 33%.
ASIPP’s recommendations build upon previous analyses from MedPAC, CMS, OIG-HHS, and the CBO. The largest projected savings are expected to result from proposed reforms to the Medicare Advantage program exceeding 120 billion per year. Exceeding 120 billion per year, with an estimated savings from specific changes which include:
· Cancellation of the proposed 4.3% payment increase for 2026:
$21 billion per year, or $210 billion over 10 years
· Elimination of payments for veterans already covered by VA insurance:
$15 billion per year, or $150 billion over 10 years
· Ending favorable selection practices: $44 billion per year, or $440 billion over 10 years
· Reforming risk adjustment mechanisms:
$40 billion per year, or $400 billion over 10 years
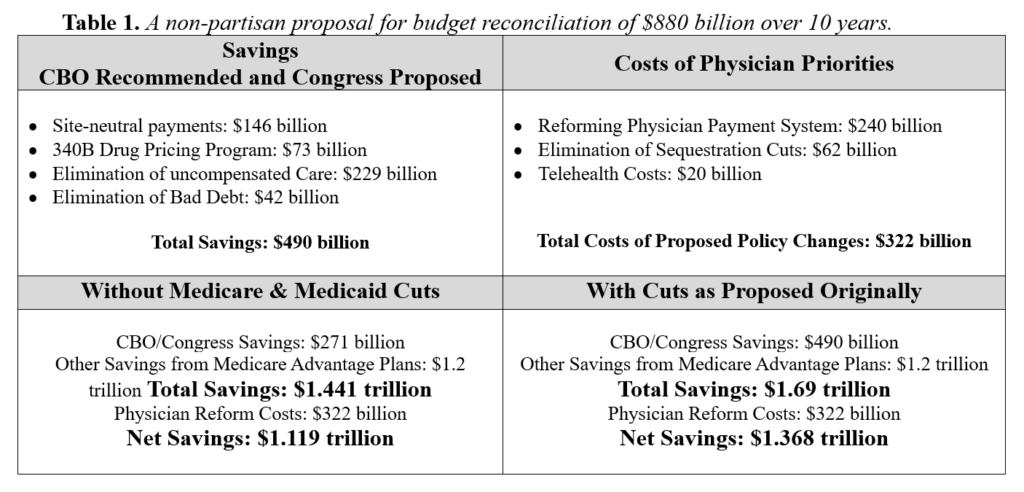
Collectively, these measures would generate an estimated $120 billion in annual savings from the Medicare Advantage program—totaling $1.2 trillion over a 10-year period.
Click here for the full 48-page Budget Reconciliation proposal. Please consider sending a PAC contribution using the following link: Click HERE to contribute to the ASIPP-PAC.
We cannot emphasize strongly enough how important your contributions are to the work we do toward the preservation of healthcare and especially interventional pain management.
ASIPP Responds to Damaging BMJ Publications Threatening Patient Access to Interventional Spine Care
The American Society of Interventional Pain Physicians (ASIPP) expresses grave concern regarding two recent publications in the British Medical Journal (BMJ) that risk significantly limiting patient care and choice in the management of chronic non-cancer spine pain.
- Letter from ASIPP President, Christopher Gharibo, MD
- Letter from ASIPP Chairman of the Board and CEO Laxmaiah Manchikanti, MD; ASIPP President-Elect Mahendra Sanapati, MD; and Academic Director, Joshua Hirsch, MD
- Formal withdrawal request
To continue this vital conversation, ASIPP will host a dedicated one-hour session at its 2025 Annual Meeting in Orlando. The session will take place on Saturday, May 17, and will be co-chaired by Dr. Christopher Gharibo and Dr. Nick Knezevic. It will include a 30-minute panel discussion with panelists: Alaa Abd-Elsayed, MD; Salahadin Abdi, MD, PhD; Sheri Albers, DO; Alexander Bautista, MD; Miles Day, MD; Shravani Durbhakula, MD; Alan Kaye, MD, PhD; Sean Li, MD; Laxmaiah Manchikanti, MD; Deborah Tracy, MD; Vinita Singh, MD; and Michael Schatman, PhD. ASIPP invites all to attend this important session. Register here.
ASIPP Advocacy Update: ASIPP Recently Met with Congress to Advocate for Several Critical Issues, Including the Extension of Telehealth Services
We want to update you on our recent visit to Washington where several ASIPP members met with key members of Congress, in both the House and Senate.
We advocated for several critical issues, including the extension of telehealth services. While we were unable to secure a permanent extension, we successfully obtained a six-month extension and will continue working for a long-term solution. Additionally, we are making progress on fraud and abuse legislation which will soon be ready for introduction.
We are also working to eliminate the recurring two-percent sequester cut and address abuses in Medicare in Medicare Advantage Plans.
Finally we discussed coverage for Peripheral Nerve Stimulation and emerging CPT coding challenges. We will be sending you a letter soon regarding ASIPP’s advocacy efforts. We encourage you to join us in these important initiatives.
BREAKING NEWS: Bill Passes House for Telehealth Provisions – Senate Must Approve for a 6-Month Extension
Through ASIPP’s extensive advocacy efforts, we were successful in getting language included in the continuing resolution to fund the government through September. This resolution would extend telehealth provisions for another 6 months.
The bill passed in the House on Wednesday while the ASIPP group was still on Capitol Hill. It appears that the extension is working its way through the Senate for approval. We are encouraged, but it has not yet been finalized.
While this is a temporary measure, our focus remains on securing a long-term solution. Many members of Congress and the Senate are advocating for a more permanent extension, ideally lasting 5 to 6 years or longer. ASIPP will continue pushing for this critical advancement.
We will provide further updates on our Capitol Hill visits and ongoing advocacy efforts soon.
BREAKING NEWS! Pain Medicine Case Reports journal has been accepted for inclusion in MEDLINE and PubMed
The American Society of Interventional Pain Physicians is excited to announce that Pain Medicine Case Reports journal (eISSN 2768-5152) has been accepted for inclusion in MEDLINE and PubMed, the prestigious bibliographic database of the U.S. National Library of Medicine. Pain Medicine Case Reports, a companion publication to the prestigious Pain Physician journal by ASIPP, joins its counterpart in achieving indexing in both MEDLINE and PubMed, marking ASIPP’s dual presence in these renowned databases.
The inclusion of Pain Medicine Case Reports journal in MEDLINE signifies a higher level of selectivity, as MEDLINE consists of the top 5,200 biomedical journals. This indexing also means that articles from Pain Medicine Case Reports will be searchable using NLM Medical Subject Headings (MeSH terms) and other metadata.
The selection for MEDLINE follows a rigorous evaluation process by reviewers from the Literature Selection Technical Review Committee (LSTRC). According to their criteria, the scientific quality of a journal’s content is the primary factor considered for indexing.
We extend our congratulations to the Pain Medicine Case Reports Editor-in-Chief, Deputy Editor-in-Chief, Journal Team, and Editorial Board for this achievement, which underscores the significance and excellence of this esteemed journal.
EXTREMELY IMPORTANT NEWS! Telehealth Changes in the Final Rule 2025 of Physician Payments CMS-1807-F and CMS-4201-F5
Thank you for your attention and participation in various activities in protecting medical practices.
We want to bring to your attention critical issues affecting patients across the United States, including those covered by Medicare, Medicare Advantage, Medicaid, and commercial insurers.
The Medicare Final Rule has significantly changed the provision of telehealth services. Starting April 1, 2025, most telehealth services will require patients to be physically present in an office or medical facility located in a rural area. This restriction excludes patients in non-rural areas from accessing telehealth services altogether. Even for those in rural regions, traveling to a designated facility can be extremely difficult, undermining one of telehealth’s primary benefits—providing care from the patient’s home. These changes will impose substantial transportation costs, create burdens for elderly patients who cannot drive, and disrupt the working population that relies on telehealth for accessible care. Currently, approximately 20% of patients depend on telehealth services.
Furthermore, if this rule remains in place, Medicare Advantage, Medicaid, and commercial insurers are expected to adopt similar policies, likely with reduced reimbursements. This will effectively dismantle telehealth services, severely limiting patient access to essential health services.
This issue is crucial for millions of patients across the country, and we hope you will take action to help preserve access to these vital services. We urgently request you to contact CMS and members of Congress (House and Senate).
Please go to VoterVoice and from there, send your letters. You may also copy the letter into your own letterhead or e-mail it directly. We have created a sample letter for your convenience.
Peripheral Nerve Stimulation
Guidelines Available!
The Evidence-Based Clinical Guidelines for the Use of Implantable Peripheral Nerve Stimulation in the Treatment of Chronic Pain from ASIPP are now available! This 92-page publication includes 374 references, 20 tables (plus 8 appendix tables), and 9 figures.
These guidelines support the use of implantable peripheral nerve stimulation leads and neurostimulators in patients with moderate to severe chronic pain refractory to two or more conservative treatments, and aim to optimize patient outcomes and promote health equity through the integration of PNS technology in clinical practice.
Find the full updated guidelines here.
CMS Releases Final 2025 Fee Schedule
CMS has finalized the 2025 Medicare Physician Fee Schedule, implementing a 2.83% cut to Medicare physician reimbursements, as previously outlined.
This cut continues a long trend of decreased reimbursements, originating with the Budget Control Act of 2011 under the Affordable Care Act. As a result, sequester cuts of 2% will remain in effect until 2032 unless Congress enacts a permanent fix to prevent these annual adjustments.
Impact on Interventional Pain Management (IPM) Services:
The final schedule reflects a 2.83% reduction in reimbursements for IPM services.
New Bipartisan Legislation Introduced to Counter Cuts:
Congressman Greg Murphy, M.D., has introduced a bipartisan bill to address this issue. This legislation aims to prevent the proposed reimbursement cut and introduce a payment increase (1.8%) equal to half of the Medicare Economic Index, aligning with recommendations from the Medicare Payment Advisory Commission.
The bill has garnered support from AMA, numerous organizations, including ASIPP. We encourage all members to act by contacting your congressman and senators to support this legislation.
ASC:
There are no major changes for IPM procedures in ASC settings, aside from adjustments in specific codes. Notably, there is a 2% to 3% increase for codes 62361, 62360, 61885, 64590, and 62362, while codes 63688, 64595, 63664, 64585, 63662, 64569, 62350, and 64553 will see a 5% to 7% decrease.
New ICD Codes Effective October 1, 2024
The new ICD-10 codes, effective October 1, 2024, must be implemented immediately to ensure proper reimbursement, including for UDS claims.
The following new codes have been developed:
M51.360: Other intervertebral disc degeneration, lumbar region with discogenic back pain only
Other intervertebral disc degeneration, lumbar region with axial back pain only.
M51.361: Other intervertebral disc degeneration, lumbar region with lower extremity pain only
Other intervertebral disc degeneration, lumbar region with leg pain only.
Other intervertebral disc degeneration, lumbar region with referred sclerotomal pain only.
M51.362: Other intervertebral disc degeneration, lumbar region with discogenic back pain and lower extremity pain
Other intervertebral disc degeneration, lumbar region with discogenic back pain and leg pain.
Other intervertebral disc degeneration, lumbar region with axial back pain and referred sclerotomal pain.
M51.369: Other intervertebral disc degeneration, lumbar region without mention of lumbar back pain or lower extremity pain
Other intervertebral disc degeneration, lumbar region without mention of lumbar back pain or leg pain.
Other intervertebral disc degeneration, lumbar region, NOS.
M51.370: Other intervertebral disc degeneration, lumbosacral region with discogenic back pain only
Other intervertebral disc degeneration, lumbosacral region with axial back pain only.
M51.371: Other intervertebral disc degeneration, lumbosacral region with lower extremity pain only
Other intervertebral disc degeneration, lumbosacral region with leg pain only.
Other intervertebral disc degeneration, lumbosacral region with referred sclerotomal pain only.
M51.372: Other intervertebral disc degeneration, lumbosacral region with discogenic back pain and lower extremity pain
Other intervertebral disc degeneration, lumbosacral region with discogenic backpain and leg pain
Other intervertebral disc degeneration, lumbosacral region with axial back pain and referred sclerotomal pain
M51.379: Other intervertebral disc degeneration, lumbosacral region without mention of lumbar back pain or lower extremity pain
Other intervertebral disc degeneration, lumbosacral region without mention of lumbar back pain or leg pain
Other intervertebral disc degeneration, lumbosacral region, NOS
M54.5: Low back pain
Excludes1: intervertebral disc degeneration, lumbar region with discogenic back pain only(M51.360)
intervertebral disc degeneration, lumbosacral region with discogenic back pain only(M51.370)
M54.3: Sciatica
Excludes1: intervertebral disc degeneration, lumbar region with lower extremity pain only(M51.361)
intervertebral disc degeneration, lumbosacral region with lower extremity pain only(M51.371)
M54.4 Lumbago with sciatica
Excludes1: intervertebral disc degeneration, lumbar region with discogenic back pain and lower extremity pain (M51.362)
intervertebral disc degeneration, lumbosacral region with discogenic back pain and lower extremity pain (M51.372)
However, these codes have not been updated with Medicaid, etc. Consequently, for facet joint pain the codes remain M47.816 and M47.817.
Similarly for radicular pain, lumbar radiculitis, M51.16 and M51.17 will remain.
See the following link to CMS: https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleid=56818&ver=45&=
Updated Antithrombotic Guidelines Available!
The updated Antithrombotic Guidelines from ASIPP are now available! This 94-page publication includes 412 references, 23 tables, and 15 figures, and offers crucial insights based on extensive research.

Extension of Telehealth Modernization Act of 2024
The Telehealth Modernization Act of 2024, a bipartisan, bicameral legislation, is progressing through Congress, which includes the following:
- Extension of certain telehealth flexibilities removing geographic requirements and expanding origination sites for telehealth services and extending them through the end of December 31, 2026 (was scheduled to expire 12/31/2024).
- This legislation also allows and extends audio only telehealth services, through December 31, 2026 (was scheduled to expire 12/31/2024).
This is great news for patients and providers to maintain access, convenience and to provide cost effective established evaluation and management services. The legislation has been sponsored by bipartisan members of Congress. If you recall, Dr. Larry Bucshon, a member of the Committee on Energy and Commerce and Congressman James Comer, Chairman of the Committee on Oversight and Accountability, discussed this extensively and worked on extending it further. While ASIPP has spearheaded to make this a reality, numerous organizations have worked tirelessly led by AMA.
The only deficiency is that it is not yet permanent. We will continue to work on this issue.
Join the AMA or Renew Your Membership Today!
On behalf of the Board of Directors of the American Society of Interventional Pain Physicians (ASIPP), we ask that you help IPM to maintain a voice in the AMA. Please join the AMA or renew your membership today.
ASIPP previously had two positions in the House of Delegates (HOD), however we just learned that in our 2024 review, we did not have enough ASIPP members on the AMA roster to keep our second seat. Consequently, we now have only one position.
However, it is now time for our 5-year review of our membership AMA match. The member list we send to the AMA every five years is the list they use each year for five years to determine our status. This means that if we fall below the minimum requirement, we stand to lose our only remaining seat.
For ASIPP to retain our seat, the AMA requires that 20% of ASIPP’s physician members also be members of the AMA. ASIPP must submit our member list no later than Monday, April 15. Because of this, we ask that you check your AMA status and renew or join TODAY.
Joining the AMA will strengthen our specialty’s representation at the national level through the AMA HOD the AMA’s policymaking body, and strengthen our ability to meet the challenges in health care today with thoughtful, well-organized responses to issues such as Medicare payment cuts, medical liability reform, etc.
Membership also gives you access to a broad range of practice management resources and award-winning publications, such as the Journal of the American Medical Association, AMNews, AMA Morning Rounds and the Archives journals.
Please support the critical activities of ASIPP by joining the AMA today. To join or renew the AMA, click on the following link: Join or Renew Here.
ASIPP UPDATES
ASIPP is pleased to announce the publication of the Comprehensive Evidence-Based Guidelines for Epidural Interventions in the Management of Chronic Spinal Pain. In preparation of the guidelines, an extensive literature review was performed. The 210-page guidelines contains 33 figures, 48 tables, 1,345 references and has 60 authors.
In addition to the review of multiple manuscripts in reference to utilization, expenditures, anatomical and pathophysiological considerations, pharmacological and harmful effects of drugs and procedures, for evidence synthesis, we have included 47 systematic reviews and 43 RCTs covering all epidural.
[ READ MORE ]
ANNOUNCEMENTS
[ INFORMATION | APPLICATION ]

[ MENTOR FORM | MENTEE FORM ]

[ CLICK TO VIEW ]
We are pleased to invite you to the ASIPP DocMatter Community, an exclusive, private platform designed to connect ASIPP members in a collaborative and secure environment. Engage with peers, discuss clinical cases, share research, and stay informed on the latest in interventional pain management.
[ CLICK TO JOIN ]
Doctor Finder allows you to search for an ASIPP® Member Interventional Pain Physician anywhere in America by name or by location. It’s quick and easy.
Since this malpractice insurance program officially launched in November 2018, ASIPP has signed up hundreds of providers with an average savings of 30%. This is professional liability insurance tailored to our specialty and will stand up for us and defend our practices.
Curi is a full-service advisory firm that serves physicians and their practices. Their valued advice is grounded in your priorities and elevated in your outcomes. They are driven by a deep understanding of your specific circumstances in medicine, business, and life. To read a few important points to keep in mind about the program, including discounts, administrative defense, cyber coverage, aggressive claims handling, and complimentary risk management CME activities, click here.
PainExam is proud to announce that it now offers preparation for the ABIPP Pain Management Board Exam! In addition, PainExam has now collaborated with ASIPP to offer Virtual Learning programs.
[ READ MORE ]
PainCast, the pain management network, has collected years worth of information on the history and processes of the pain management specialization and transformed it into a virtual library of videos, journals, articles, podcasts, and more – all at your fingertips.
Leading experts in their respective fields contributed chapters on specific topics to present a cogent and integrative understanding of the field of regenerative medicine as applicable for interventional pain physicians.
[ READ MORE ]
This comprehensive review covers the full and latest array of interventional techniques for managing chronic pain and features new chapters covering challenges with opioid therapy, impact of COVID-19, and spinal interventional techniques.
[ READ MORE ]
ASIPP has formed a partnership with Henry Schein and PedsPal, a national GPO that has a successful history of negotiating better prices on medical supplies and creating value added services for the independent physician.
[ READ MORE ]
ASIPP is now offering our members the benefit of a unique revenue cycle management/billing service. We have received a tremendous amount of interest in the ASIPP billing and coding program.
[ READ MORE ]